Blog Archives
The Missing Millions: Why So Many Veterans Still Lack Disability Ratings
In the United States today, a significant portion of the veteran population remains without a service-connected disability rating—even though many receive ongoing care from the Department of Veterans Affairs (VA). This gap affects millions and stems from long-standing structural issues and common misunderstandings.
How Many Veterans Are Unrated?
Recent federal data shows:
17.8 million veterans currently live in the U.S.
Only 5.2 million (about 30%) have a service-connected disability rating.
That leaves roughly 12.5 million veterans without a rating, including an estimated 6 million who separated before disability assessments became part of the mandatory out-processing process.
Before the mid-1990s and early 2000s reforms, the DoD did not require a disability evaluation as part of separation or retirement. Millions of veterans left service with no assessment and never filed later simply because the process was unclear or unknown.
Two VA Systems — and They Don’t Communicate
A critical fact many veterans do not know:
VA Healthcare and VA Disability Compensation are completely separate systems.
Receiving VA medical care does not create or update a disability rating.
Diagnoses, imaging, or treatment inside VA healthcare records are not reviewed for disability compensation unless a veteran files a claim.
No condition—primary or secondary—moves into the disability system automatically.
Many veterans assume that being treated for chronic pain, orthopedic injuries, sleep issues, or mental health conditions means their disability file is being updated. It isn’t. Only a formal claim triggers review.
The Impact on Veterans
Millions of veterans who never filed a claim at all.
Veterans with worsening conditions who never requested rating increases.
VA healthcare patients with serious diagnoses that were never evaluated for service-connection.
Missed compensation, lost benefits, and reduced access to programs tied to rating thresholds.
A single misconception—“VA healthcare updates my disability rating”—can cost a veteran years of deserved benefits.
What Every Veteran Should Do Now
To ensure disability benefits reflect current health conditions, veterans should:
1. Review their conditions regularly
Check for new diagnoses, worsening symptoms, or secondary conditions.
2. File new or supplemental claims
Use VA.gov, mail, or accredited submission channels to request evaluation.
3. Understand the system
VA healthcare records do not update disability ratings. A claim must be submitted.
4. Track secondary conditions
Issues like sleep apnea, depression, migraines, radiculopathy, GERD, or joint degeneration often stem from service-connected primaries.
Veterans who separated before mandatory disability evaluations around 2010 are especially vulnerable because many were never informed of the modern process.
Closing the Gap
With only ~30% of veterans holding a disability rating—and millions eligible but unrated—awareness is essential. Understanding that VA healthcare and VA disability compensation operate independently is the first step toward ensuring every veteran receives the benefits they earned through service.
Need Help Understanding Your Claim Path?
If you or a veteran you know is unsure about eligibility, secondary conditions, or how to properly file, guidance is available. Filing a claim is not automatic—but it can be straightforward when you understand the rules and requirements.
A Journey to Acceptance: My Eye-Opening Experience with Medical Marijuana
I was born and raised in Miami, Florida — in the middle of chaos and change. The city I grew up in during the 70s and 80s was a powder keg of race riots, refugees, and drugs. Miami was overrun — and that’s putting it kindly. Cocaine, marijuana, and the war on drugs were everywhere.
I never touched any of it. Not once.
It was a badge of honor, a personal vow. My father was a judge, and I took pride in the discipline that kept me away from substances that, to me, represented weakness and failure. I saw alcohol as adult, social, and controlled. Marijuana? That was for the lost.
For most of my life, I never questioned that belief.
But life has a way of testing the walls we build around our certainty.
When my wife’s illness began to take over our nights, sleep became hard. She was in constant pain, and nothing — not the pills, not the prescriptions, not the endless “next options” — brought her relief without a cost. Then one night, she tried a simple gummy. She slept through the night.
That experience made me aware — painfully so — of my own hypocrisy. While she found healing through a plant I had long dismissed, I was numbing myself each night with alcohol — not to enjoy, but to stop feeling, to force sleep. I told myself it was normal, acceptable, even earned. But it wasn’t helping.
It wasn’t until I was helping a client — a veteran — through her VA disability claim that the truth caught up with me. She confided in me about her fear of admitting she used marijuana to manage anxiety and sleep. I told her what I believed: that she shouldn’t be ashamed, that seeking help isn’t weakness, and that medical care, when legal and responsible, is private and protected.
Then it hit me like a mirror.
How could I coach her toward honesty and healing while denying myself the same?
That same day, I called my wife’s physician, scheduled an appointment, and applied for my medical marijuana card. Since then, I take a gummy every night. I sleep. I think more clearly. I drink less. I feel present.
My view has changed completely — not because of politics or persuasion, but because of experience. What I once called weakness, I now see as wisdom. The real weakness was refusing to see past my own judgment.
In Florida, medical marijuana has been lawful since 2016. But for me, it only became personal when life humbled me enough to listen.
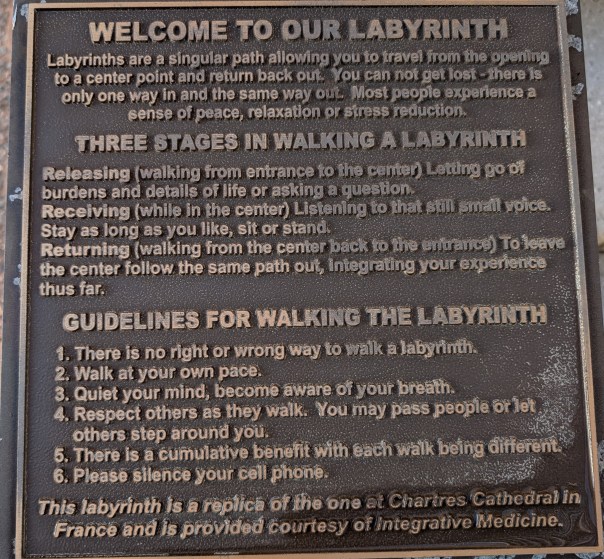
The more I experience life, the more I understand that nothing truly changes until we become aware. Awareness brings empathy, and empathy brings wisdom. And wisdom — I’ve learned — is not the privilege of youth, but the product of life lived honestly.
What will my life be like in 3 years?
I dare not answer the question.
That was my first response when someone asked where I see myself in three years. Without hesitation, fear stepped in — not fear of failure, but fear of imagining life beyond now. Beyond her.
Yesterday, my wife finalized her cremation plans. I’ve done this before — for my sister, for my father. Each time, it became a necessary transaction. Paperwork, signatures, polite condolences exchanged over a table that felt too small for the weight in the room. The funeral director came to the house. We completed the forms. She paid for her services. Efficient. Respectful. Businesslike.
It’s best to do this before it happens, they say — so there’s one less thing to cause anxiety and pain.
But is that really true? Or is it that I just didn’t want to do this again?
Because the truth is, no matter how many times I’ve faced loss, I still don’t know how to prepare for it. I can manage logistics, but not emotions. I can sign the papers, but not the permission slip to move forward.
When I think about the future — traveling, my children, my new grandbaby — I feel guilty. There’s a horrible tension between the yearning to be free and the desperate wish for this stage of life to never end. How do you reconcile wanting relief and wanting permanence at the same time?
Maybe that’s what being human really is — living inside the contradiction.
We spend our lives trying to control time, plan for tomorrow, build systems, write goals. But life keeps reminding us it doesn’t belong to us. It moves with or without our consent.
Three years from now, I don’t know where I’ll be. Maybe I’ll be standing somewhere new, lighter but not the same. Maybe I’ll still wake up some mornings expecting to hear her voice. Maybe I’ll finally find a kind of peace in the not-knowing.
Because the truth is, none of us can control life. We can only honor it
Where will I be in 3 years…..
It Takes a Village: The Realities of End-of-Life Care
Yesterday was one of the hardest days yet. My wife, Sherri, whispered that she wished for death. Her pain was unbearable, even through layers of medication. Her bed sore reopened, two abscesses formed in her mouth, and the ache from her brittle bones and unhealed surgical site—after eight surgeries, two wound vacuums, and countless antibiotics—was relentless.
We took her to the dentist, who could do little more than write a referral to an oral surgeon. In that moment, I realized what Sherri already knew: sometimes, the course of care no longer offers a path worth taking. The procedures, the pain, the waiting—none promise comfort or meaningful recovery.
Yet, it takes a village. Her sister, her cousin, and her circle of friends have become our lifeline. Their presence gives her strength. She lights up when they visit, laughs, and feels alive again. But the cost is steep—those moments of joy are followed by hours of exhaustion and pain. Now, every visit, every appointment must be weighed against what it will take from her.
I see couples in the hospital—older than us—one sick, one trying to navigate the maze of care while barely able to support themselves. Too often, they end up alone in nursing homes, fading quietly. I’m grateful I’m still strong enough to help Sherri, even if I know there will be a toll later.
End-of-life care isn’t about heroics or procedures—it’s about presence. It’s about conserving what’s left of the body’s strength and surrounding the spirit with love. The truth is, medical science can extend life, but only community—family, faith, and friendship—can make it worth living.
The Front Lines of Cancer
Yesterday, we reached acceptance. Not surrender — not quitting — but an understanding: this cancer is incurable. It continues to spread slowly, like a snake coiling itself around its prey.
And yet, in the middle of it all, there is beauty.
Our youngest is in high school now. She wakes up on her own, gets ready, eats breakfast. She is excited about life. She’s playing lacrosse, wants to go to practice, wants to do well in school. It’s such a good time.
The other night, my wife told her that she wanted her to have her wedding ring. Tears came, but then laughter too, as our daughter said it was too small for her finger. Somehow, the moment turned to a joke about making it into a “grill” for our dog with the terrible underbite. This is life and love — sorrow and laughter tangled together.
This weekend, our oldest came home. She’s about to start graduate school after years of working. She asked her mother, “Are you going to die?” My wife, steady as ever, said: “I will — but I don’t intend to do it soon. You need to go to graduate school and live your life. This is your dream. Keep going.” Then she gave her the diamond pendant we had made from her mother’s stone. They cried for hours.
One of our sons is getting married in October and then heading into the military. We already have our plane tickets and hotel. No setbacks. We will be there. We’ve become experts in travel planning and stress mitigation, as Sherri can only manage about two hours of chair time a day. No setbacks — we so want to be there.
And then there’s our granddaughter. Just 18 months old, already going down slides. We watched the video of her laughing all the way, and it filled us with joy.
It is a wonderful time.
That might sound strange to say, but it’s true. In these trying days, every moment of laughter, every milestone, every piece of ordinary life feels even more precious. The weight of suffering sharpens the beauty of joy. And when you know that time is short, you hold tighter to the moments that matter most.

Every morning, I bring her breakfast in bed
Every morning, I bring her breakfast in bed. Whatever she wants—peanut butter on a waffle, an apple, crispy bacon, a bowl of raisin bran, sous ve eggs—I make it. Most days, she’ll stick to the same thing for days, even weeks. It’s a small thing, but it’s the least I can do for all she endures.
She can’t walk anymore. The electric wheelchair gives her about an hour and a half of mobility before the pain forces her to lie down. The cancer has spread to her bones. Yet, somehow, she still smiles. She still refuses to give up.
Breakfast has always been my favorite meal. Now its much more than that, its a check in with a smile still here.

Two Hours for a Shower—And a Lifetime of Love
Today it took two hours to help my wife, take a shower in our own home.
Two hours of lifting and moving, of prepping and adjusting.
Unhooking her IV.
Unwrapping layers of dressings and wound care.
Lining the shower with towels and placing the chair just right.
Washing her hair, combing it gently.
Finding clothes that work for a body in pain.
Changing the linens, warming the room, preparing her toothbrush—preloaded with toothpaste because her hands don’t work anymore.
Two hours of effort.
For 30 minutes of normalcy.
For 10 minutes of comfort.
For one more moment of feeling clean and human.
And then back to bed, with the “bear hugger” blowing warm air to keep her body from freezing. Her body can’t regulate temperature anymore.
She smiled when it was over.
But she’s tired.
I’m tired.
And tomorrow… she faces her third surgery in just 60 days.
We had held on to hope that she could go on the family trip to Japan—something she’s been dreaming of for a year. But this new surgery means she’ll stay behind, once again watching life from the sidelines of recovery.
That’s what cancer does. That’s what infection does. That’s what caregiving is.
It takes things—quietly, relentlessly.
It takes time, energy, tears, sleep, plans, dreams, vacations, strength.
But we keep giving. Because love gives.
I won’t give up hope.
Not today.
Not tomorrow.
Not on her.
She’s still here. Still smiling through it. Still fighting. Still loving us in her own quiet way.
So we’ll keep going.
One day at a time.
One shower at a time.
One breath at a time.
Because this is what love looks like when it’s on the battlefield.
The Power of Presence: How to Support Caregivers
When someone you love is gravely ill or bedridden, the world becomes very small. The walls of the home close in. Time slows. Days blur together. Both the person being cared for—and the caregiver—begin to live in a kind of suspended animation, where joy, spontaneity, and connection are replaced by routine, worry, and waiting.
People often ask, “What can I do?”
And it’s a sincere question. They want to help. So they send flowers. Cards. Food. Gift cards. And all of those are kind gestures. All of them are appreciated.
But if you really want to help a caregiver—and the person they’re caring for—be present. Show up.
Caregiving is not just physically exhausting. It’s emotionally isolating. The one who is ill is often trapped in their body, in their symptoms, in a bed they can’t escape. The caregiver, meanwhile, is trapped in responsibility, routine, and quiet desperation.
Isolation is the great thief.
It steals joy, perspective, and sometimes even hope. But when someone walks through the door just to be there, everything changes—even if only for a little while.
Here’s what you may not see:
When visitors come over, something shifts.
The house feels lighter.
The person being cared for suddenly wants to sit up straighter, to smile, to tell stories—even if they can’t move or speak much.
The caregiver may finally exhale, just a little.
You don’t need to bring anything. Just your presence. A shared moment. A hand held. A joke told. A prayer whispered.
It’s not about what you do. It’s about that you came.
We often overcomplicate compassion. We think we need the “right” thing, the perfect timing, or something polished and proper.
But love isn’t complicated.
Compassion shows up unannounced and says, “I’m here.”
It’s the ministry of presence.
So, if you’re wondering how to help:
- Visit. Even 15 minutes can be sacred.
- Sit. Watch a show, listen to music, share a memory.
- Talk. About something—anything—besides illness.
- Listen. Sometimes just being a witness to the struggle is a gift.
- Stay connected. Don’t let their world shrink without a fight.
Because at the end of the day, love looks like presence. And presence heals in ways medicine can’t.

Understanding Anticipatory Grief as a Caregiver
I’ve spent a lifetime wearing uniforms — first in the military, then in business — but no uniform could have prepared me for the one I wear now: caregiver.
My wife is still here. She still smiles. Still laughs. Still says “I love you” with the same strength that got her through childbirth without a scream and once drove a screwdriver bit through her hand with nothing more than a calm “ouch.” But even with all that strength, I know what’s coming. And somewhere along the way, I realized I was already grieving.
It wasn’t denial that kept me from seeing it; I saw every scan, every new medication, every tear. It wasn’t anger that overwhelmed me, though I’ve certainly felt flashes of frustration — at broken systems, unanswered prayers, and my own helplessness. It was something quieter. Slower. A gradual ache of knowing that the woman I love is slipping away in pieces.
That’s what anticipatory grief is — mourning someone while they’re still alive. It’s showing up with love and purpose even as the shadows grow longer. It’s grieving not just the final goodbye, but the thousands of little ones along the way: the goodbye to traveling together, to her independence, to her baking and cooking in the kitchen.
I’ve come to understand that the five stages of grief — denial, anger, bargaining, depression, acceptance — aren’t a straight road. They’re more like a roundabout we circle again and again. And while Kübler-Ross introduced them to describe how patients face terminal illness, caregivers like me feel them too — just in advance.
Right now, I live somewhere between acceptance and heartbreak. I’ve accepted what’s coming. But each day, I still fight to create joy, dignity, and presence. We watch movies in the car so she doesn’t have to get out. We eat takeout in the bed because she cant sit at the table. I hold her hand not just in sickness, but in the holy weight of being here — now.
If you’re walking this road too, know that grief doesn’t wait for death. And love doesn’t wait for perfection. You are doing holy work, even when your hands feel empty.
Let yourself grieve. But also — let yourself love, fiercely, while there’s still time.

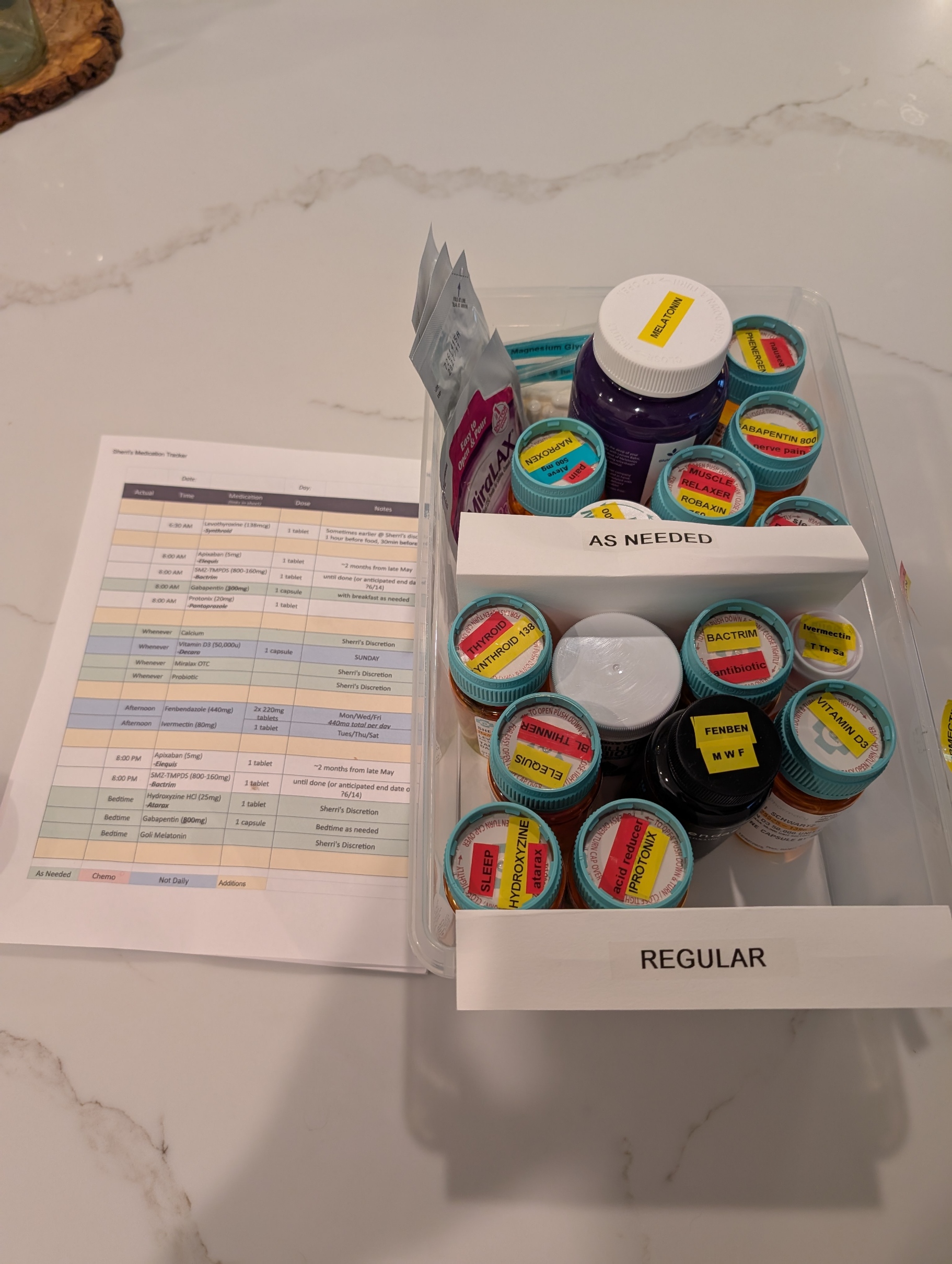
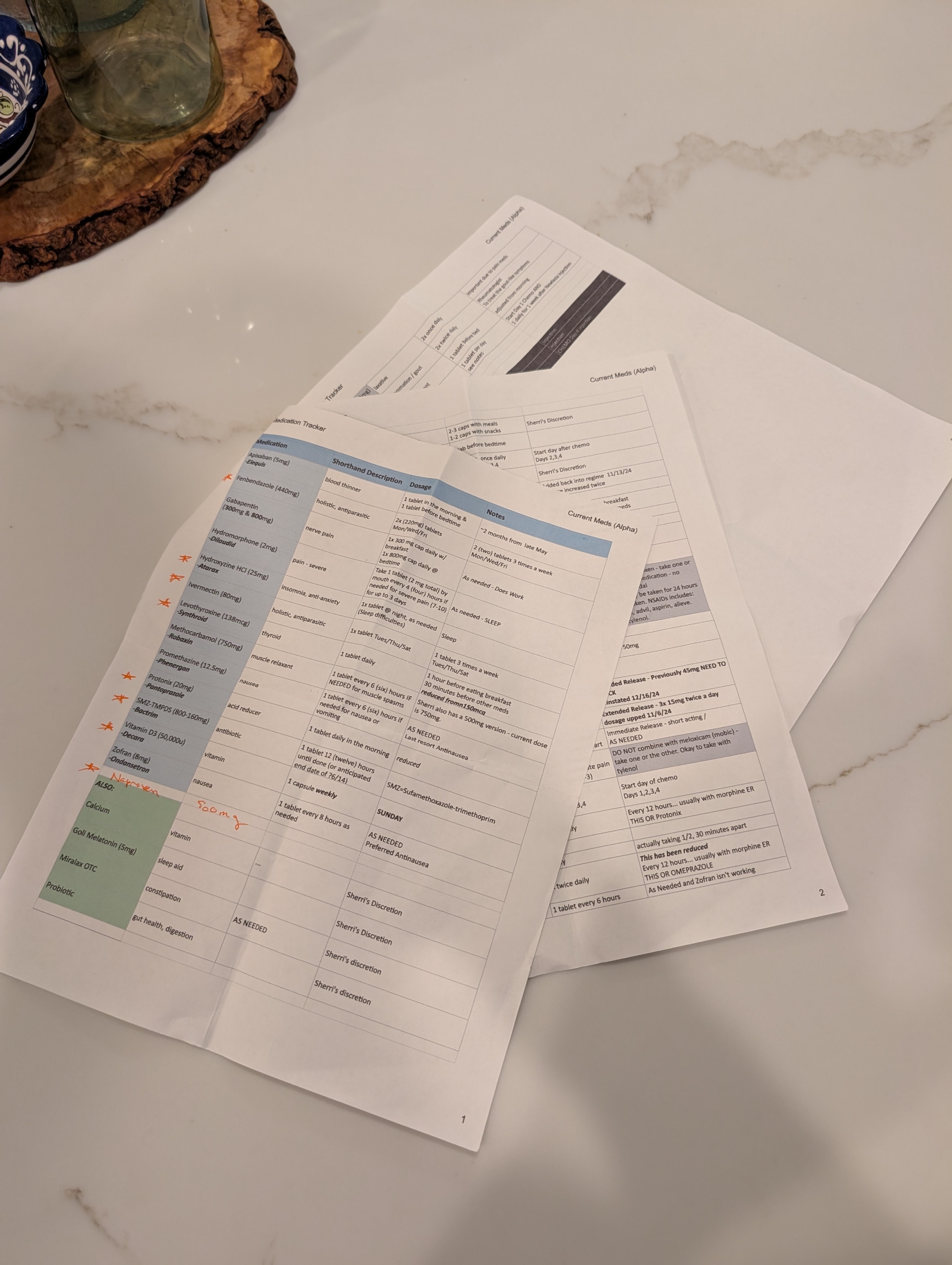
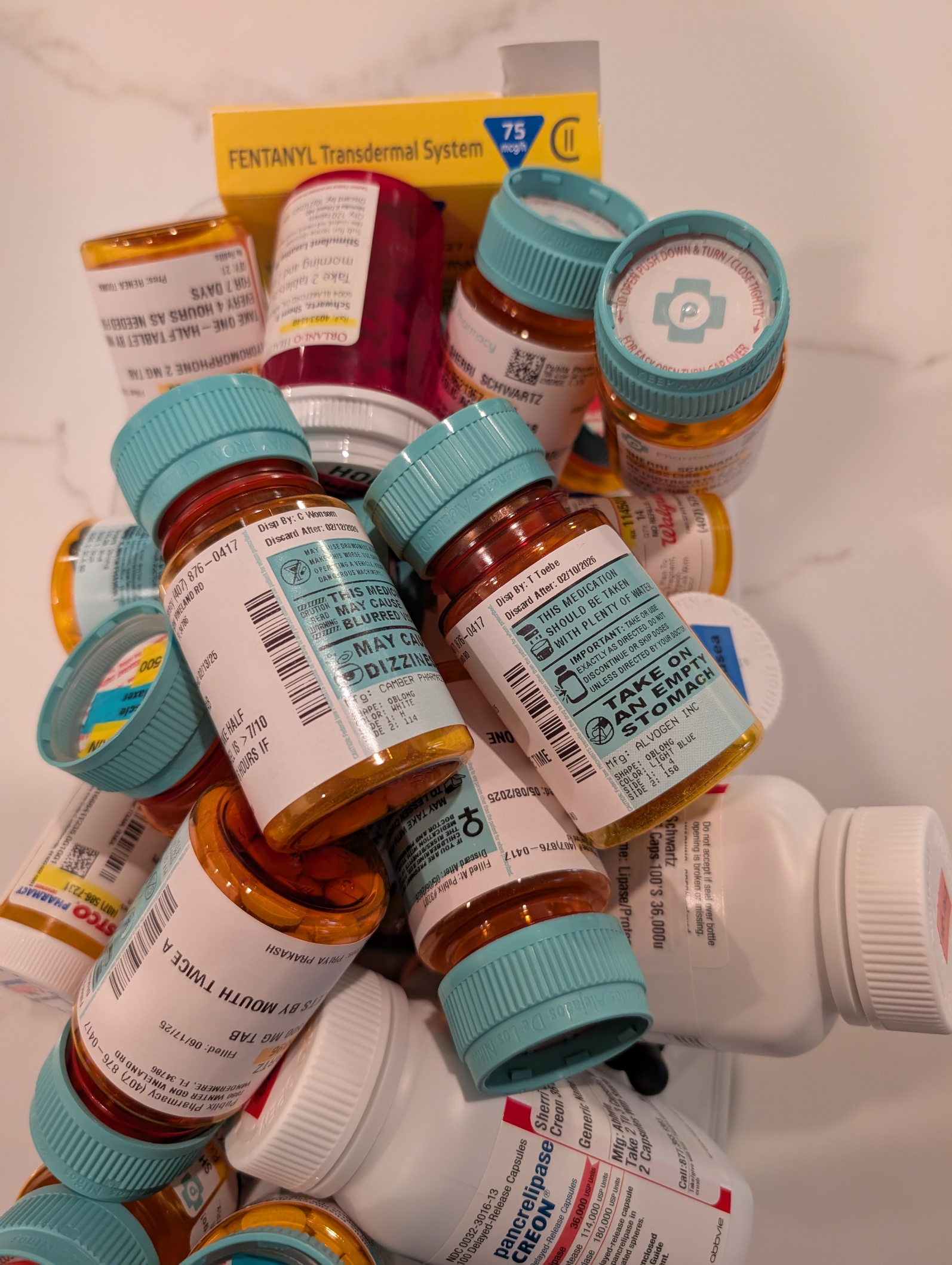
Pills, Pills, and More Pills: The Hidden Burden of Complex Caregiving
One of the most overwhelming challenges in being a caregiver to a loved one with complex health needs is managing medications. It’s not just about handing over a pillbox. It’s navigating a labyrinth of prescriptions from multiple providers—some within the same healthcare system, others outside it, and even some who are technically in the system but don’t have credentials to see each other’s records. The result? A fragmented network of well-meaning professionals relying on the patient or caregiver to connect the dots.
Every outpatient visit starts with the same question: “Are you still taking…?” And if your loved one isn’t completely lucid or you’re not fully dialed in 24/7, the answer might not be accurate. That’s when the real risk begins. Medications get missed, taken at the wrong time, or worse—interact dangerously. Even with tools like MyChart and pharmacy alerts, medication management for multi-disciplinary patients is a full-time job that demands vigilance and coordination.
Thankfully, my wife has what many don’t: an extended family care team. Her sister—a brilliant organizer—maintains a shared medication log with active and retired prescriptions. Her cousin, a provider based in California, monitors her records through MyChart and flags potential issues or treatment recommendations. Their support has been nothing short of lifesaving.
As her primary caregiver, I also leaned into my background in healthcare and team leadership. I applied principles I once used to support the care for wounded or sick soldiers returning from Iraq at Fort Moore (then Fort Benning), where we built systems but more importantly had people to prevent our service members from getting lost in the shuffle. It’s painful to see that the civilian system still struggles with the same problem.
Where is the care manager? Aren’t they the quarterback? I once asked that question myself—only to be told their panel included 250 complex cases. No human can meaningfully manage that many lives. It was a sobering reminder that “the system” is overloaded, and for those without advocates, the consequences can be tragic.
Having a palliative care physician onboard has been critical. Contrary to common perception, they don’t just deal with end-of-life care. They focus on quality of life—managing pain, coordinating care, and yes, reconciling all those pills. My wife currently has more than 10 providers involved in her care. That number doesn’t include staff, specialists, or the relentless demands of insurance approvals.
Medication management isn’t glamorous, but it’s a battlefield—and like all battlefields, it requires a team, a plan, and an unwavering commitment to the person you’re fighting for. I bring my military mindset to this mission every day. And while I can’t stop the tide of prescriptions or the systemic gaps in care, I can make sure my wife never faces them alone.