Author Archives: LOUJSWZ Inc.
The Front Lines of Cancer
Yesterday, we reached acceptance. Not surrender — not quitting — but an understanding: this cancer is incurable. It continues to spread slowly, like a snake coiling itself around its prey.
And yet, in the middle of it all, there is beauty.
Our youngest is in high school now. She wakes up on her own, gets ready, eats breakfast. She is excited about life. She’s playing lacrosse, wants to go to practice, wants to do well in school. It’s such a good time.
The other night, my wife told her that she wanted her to have her wedding ring. Tears came, but then laughter too, as our daughter said it was too small for her finger. Somehow, the moment turned to a joke about making it into a “grill” for our dog with the terrible underbite. This is life and love — sorrow and laughter tangled together.
This weekend, our oldest came home. She’s about to start graduate school after years of working. She asked her mother, “Are you going to die?” My wife, steady as ever, said: “I will — but I don’t intend to do it soon. You need to go to graduate school and live your life. This is your dream. Keep going.” Then she gave her the diamond pendant we had made from her mother’s stone. They cried for hours.
One of our sons is getting married in October and then heading into the military. We already have our plane tickets and hotel. No setbacks. We will be there. We’ve become experts in travel planning and stress mitigation, as Sherri can only manage about two hours of chair time a day. No setbacks — we so want to be there.
And then there’s our granddaughter. Just 18 months old, already going down slides. We watched the video of her laughing all the way, and it filled us with joy.
It is a wonderful time.
That might sound strange to say, but it’s true. In these trying days, every moment of laughter, every milestone, every piece of ordinary life feels even more precious. The weight of suffering sharpens the beauty of joy. And when you know that time is short, you hold tighter to the moments that matter most.

Every morning, I bring her breakfast in bed
Every morning, I bring her breakfast in bed. Whatever she wants—peanut butter on a waffle, an apple, crispy bacon, a bowl of raisin bran, sous ve eggs—I make it. Most days, she’ll stick to the same thing for days, even weeks. It’s a small thing, but it’s the least I can do for all she endures.
She can’t walk anymore. The electric wheelchair gives her about an hour and a half of mobility before the pain forces her to lie down. The cancer has spread to her bones. Yet, somehow, she still smiles. She still refuses to give up.
Breakfast has always been my favorite meal. Now its much more than that, its a check in with a smile still here.

Two Hours for a Shower—And a Lifetime of Love
Today it took two hours to help my wife, take a shower in our own home.
Two hours of lifting and moving, of prepping and adjusting.
Unhooking her IV.
Unwrapping layers of dressings and wound care.
Lining the shower with towels and placing the chair just right.
Washing her hair, combing it gently.
Finding clothes that work for a body in pain.
Changing the linens, warming the room, preparing her toothbrush—preloaded with toothpaste because her hands don’t work anymore.
Two hours of effort.
For 30 minutes of normalcy.
For 10 minutes of comfort.
For one more moment of feeling clean and human.
And then back to bed, with the “bear hugger” blowing warm air to keep her body from freezing. Her body can’t regulate temperature anymore.
She smiled when it was over.
But she’s tired.
I’m tired.
And tomorrow… she faces her third surgery in just 60 days.
We had held on to hope that she could go on the family trip to Japan—something she’s been dreaming of for a year. But this new surgery means she’ll stay behind, once again watching life from the sidelines of recovery.
That’s what cancer does. That’s what infection does. That’s what caregiving is.
It takes things—quietly, relentlessly.
It takes time, energy, tears, sleep, plans, dreams, vacations, strength.
But we keep giving. Because love gives.
I won’t give up hope.
Not today.
Not tomorrow.
Not on her.
She’s still here. Still smiling through it. Still fighting. Still loving us in her own quiet way.
So we’ll keep going.
One day at a time.
One shower at a time.
One breath at a time.
Because this is what love looks like when it’s on the battlefield.
The Power of Presence: How to Support Caregivers
When someone you love is gravely ill or bedridden, the world becomes very small. The walls of the home close in. Time slows. Days blur together. Both the person being cared for—and the caregiver—begin to live in a kind of suspended animation, where joy, spontaneity, and connection are replaced by routine, worry, and waiting.
People often ask, “What can I do?”
And it’s a sincere question. They want to help. So they send flowers. Cards. Food. Gift cards. And all of those are kind gestures. All of them are appreciated.
But if you really want to help a caregiver—and the person they’re caring for—be present. Show up.
Caregiving is not just physically exhausting. It’s emotionally isolating. The one who is ill is often trapped in their body, in their symptoms, in a bed they can’t escape. The caregiver, meanwhile, is trapped in responsibility, routine, and quiet desperation.
Isolation is the great thief.
It steals joy, perspective, and sometimes even hope. But when someone walks through the door just to be there, everything changes—even if only for a little while.
Here’s what you may not see:
When visitors come over, something shifts.
The house feels lighter.
The person being cared for suddenly wants to sit up straighter, to smile, to tell stories—even if they can’t move or speak much.
The caregiver may finally exhale, just a little.
You don’t need to bring anything. Just your presence. A shared moment. A hand held. A joke told. A prayer whispered.
It’s not about what you do. It’s about that you came.
We often overcomplicate compassion. We think we need the “right” thing, the perfect timing, or something polished and proper.
But love isn’t complicated.
Compassion shows up unannounced and says, “I’m here.”
It’s the ministry of presence.
So, if you’re wondering how to help:
- Visit. Even 15 minutes can be sacred.
- Sit. Watch a show, listen to music, share a memory.
- Talk. About something—anything—besides illness.
- Listen. Sometimes just being a witness to the struggle is a gift.
- Stay connected. Don’t let their world shrink without a fight.
Because at the end of the day, love looks like presence. And presence heals in ways medicine can’t.

VA Claims Processing: Success or Hidden Challenges?
In the July 2025 newsletter, the Department of Veterans Affairs proudly announced that it had “processed” over 2 million disability claims—faster than ever before. At first glance, this milestone sounds like a tremendous success. But for veterans who have lived at the intersection of military service and medical hardship, there’s a deeper story behind the headlines.
As a veteran and someone who assists others in navigating the VA claims process, I’ve learned to read between the lines. The newsletter fails to disclose how many of those 2 million claims were denied—a critical omission that affects real lives. A high throughput of claim processing does not necessarily equate to high-quality or just outcomes for veterans.
At the same time, the VA linked to its public repository of Disability Benefits Questionnaires (DBQs) available here. These are detailed, medically technical forms that the VA encourages veterans to bring to their private providers to “expedite” claims—allegedly reducing costs and time associated with VA-conducted exams.
On the surface, this sounds like a win-win. But if you’ve filled out one of these forms or asked a doctor to complete one, you know that each DBQ is 12 to 16 pages long, highly technical, and time-consuming. It could take an experienced clinician over an hour—per form—with no reimbursement provided by the VA.
Let’s pause there: the government is asking veterans to pay out of pocket or call in favors from already overburdened civilian providers, many of whom are unfamiliar with VA language, legal thresholds, or the 38 CFR standards. These forms may reduce government costs, but they shift that burden onto the backs of those who served.
And what’s more concerning is this: Is this an unspoken gatekeeping tactic? Is the sheer complexity of DBQs and the absence of compensation for providers quietly slowing down or stalling new claims from older-era veterans—those who served between 1965 and 2015—who didn’t benefit from the digital medical records era?
As someone working daily with veterans—at the proverbial GEMBA or “point of the spear”—I’ve witnessed firsthand how the standard of approval appears to have shifted. In the first few months of this administration, P&E exams were paused for over three months. Now, adjudications seem stricter than ever. Subjective? Perhaps. But for many veterans, this feels like a regression, not progress.
Questions We Should Be Asking the VA:
- What percentage of the 2 million “processed” claims were denied, granted, or partially awarded?
- Why are providers not compensated for the time it takes to complete detailed DBQs?
- Has the standard of adjudication shifted from the traditional “at least as likely as not” (51%) burden of proof?
- Why are we not leveraging modern AI and automation tools to reduce claim burden for the veteran?
- How does the VA plan to assist older veterans—whose medical records are often incomplete or paper-based—in navigating these requirements?

AI Can’t Care – Why Human Trust Still Wins in a Tech-Driven World
In a world that feels increasingly automated, one thing is becoming clearer every day: people still crave connection. Especially when they’re hurting. Especially when they’re trying to navigate something as emotional and complex as the VA disability claims process.
At LOUJSWZ INC, we embrace technology. We use AI to make our work more efficient, more accurate. But AI is not our product. Our product is trust. And there isn’t a line of code out there that can replicate that.
I recently sat down with a fellow veteran who shared how rushed his transition was and how unsure he felt even after submitting his claim. He used the free services available to him—VFW, county VSO, mobile VA outreach—and still felt like something might have been missed. And you know what? He’s not alone. That “what did I forget?” feeling is far too common.
There are tools now that can read disability guides and recommend conditions. They’re fast. They’re free. But they don’t know how to look you in the eye and ask, “What really hurts?” They don’t hear the pause in your voice or notice the symptoms you forgot to say out loud. They don’t walk your journey. I do. I have lived it.
Porter’s Five Forces tells us that AI is shaking every industry—lowering barriers, increasing buyer power, and making substitutes more accessible. But it also tells us something else: the key to success in a competitive landscape is differentiation.
LOUJSWZ isn’t just another support service. We’re your battle buddy through bureaucracy. We know the system, yes—but more importantly, we know you. And we’re here to make sure you get what you’ve earned. No shortcuts. No automated empathy. Just people helping people, with the support of the best tools available—not the replacement of them.
Because at the end of the day, AI may shape strategy, but it’s still heart that shapes trust.

Understanding Anticipatory Grief as a Caregiver
I’ve spent a lifetime wearing uniforms — first in the military, then in business — but no uniform could have prepared me for the one I wear now: caregiver.
My wife is still here. She still smiles. Still laughs. Still says “I love you” with the same strength that got her through childbirth without a scream and once drove a screwdriver bit through her hand with nothing more than a calm “ouch.” But even with all that strength, I know what’s coming. And somewhere along the way, I realized I was already grieving.
It wasn’t denial that kept me from seeing it; I saw every scan, every new medication, every tear. It wasn’t anger that overwhelmed me, though I’ve certainly felt flashes of frustration — at broken systems, unanswered prayers, and my own helplessness. It was something quieter. Slower. A gradual ache of knowing that the woman I love is slipping away in pieces.
That’s what anticipatory grief is — mourning someone while they’re still alive. It’s showing up with love and purpose even as the shadows grow longer. It’s grieving not just the final goodbye, but the thousands of little ones along the way: the goodbye to traveling together, to her independence, to her baking and cooking in the kitchen.
I’ve come to understand that the five stages of grief — denial, anger, bargaining, depression, acceptance — aren’t a straight road. They’re more like a roundabout we circle again and again. And while Kübler-Ross introduced them to describe how patients face terminal illness, caregivers like me feel them too — just in advance.
Right now, I live somewhere between acceptance and heartbreak. I’ve accepted what’s coming. But each day, I still fight to create joy, dignity, and presence. We watch movies in the car so she doesn’t have to get out. We eat takeout in the bed because she cant sit at the table. I hold her hand not just in sickness, but in the holy weight of being here — now.
If you’re walking this road too, know that grief doesn’t wait for death. And love doesn’t wait for perfection. You are doing holy work, even when your hands feel empty.
Let yourself grieve. But also — let yourself love, fiercely, while there’s still time.

The Truth About Insurance Delays in Medical Equipment Access
Imagine this: your loved one has just been admitted to a rehabilitation hospital. She has limited mobility, use of only one hand, and is in critical need of a powered wheelchair to regain a sliver of independence. The medical team sees the need clearly. The rehab team jumps into action—generating a physician’s statement of need, identifying a qualified vendor, and aligning care planning around the use of this essential device.You would think the next step is straightforward—insurance approves, device is delivered, and your loved one can begin her recovery journey with dignity.
Wrong.
The insurance company’s response? “It will take a minimum of 60 days to process.” That’s 45 days after the patient is discharged—leaving her bed-bound or reliant on round-the-clock support in the meantime. If you want the device sooner, it’s available—but only if you can pay the full cost upfront, out of pocket.Luckily, I had just enough space on a credit card—$2,200—and I bought the chair myself. Within hours, it was delivered. The result? My wife, who was at risk of becoming isolated in her own home, regained some independence. We then submitted all the paperwork for reimbursement through the approved process—yes, still by fax in 2025. The insurance company now has 75 days to decide whether the benefit will be honored.And what if they do approve it? After deductibles, co-pays, and co-insurance calculations, they’ll only reimburse less than 50% of the total cost.This experience was frustrating, disheartening—and honestly, a little scary. What happens to people who don’t have a credit card? Who can’t float the cost while waiting months for reimbursement? Are they just expected to sit, lay, and suffer in silence?—The Business Rules Are Broken. Health insurance providers often tout their “support” for necessary medical equipment. But their business rules are built for denial, delay, and discouragement:Delays in processing—even with a signed medical necessity letter.Reimbursement after the fact, not timely fulfillment.Inadequate coverage—only partial payments after all the math. And yet, the market has made it possible to buy a power chair on the same day. The disconnect is glaring: it’s not a matter of availability, it’s a matter of access.
—Final Thoughts: This post isn’t about venting. It’s a call to advocate for change. Durable medical equipment (DME) is not a luxury—it’s a lifeline. Yet current insurance practices treat it like an optional convenience.If you’re a caregiver, patient, or family member going through this system, I see you.
If you’re a policymaker or insurance executive reading this, I urge you—align the policy to the people. Because right now, too many are being left behind.—If you’ve faced similar challenges or want to share resources that have helped you navigate the DME approval process, please share them in the comments. We need to amplify these stories and stand together for better healthcare access.

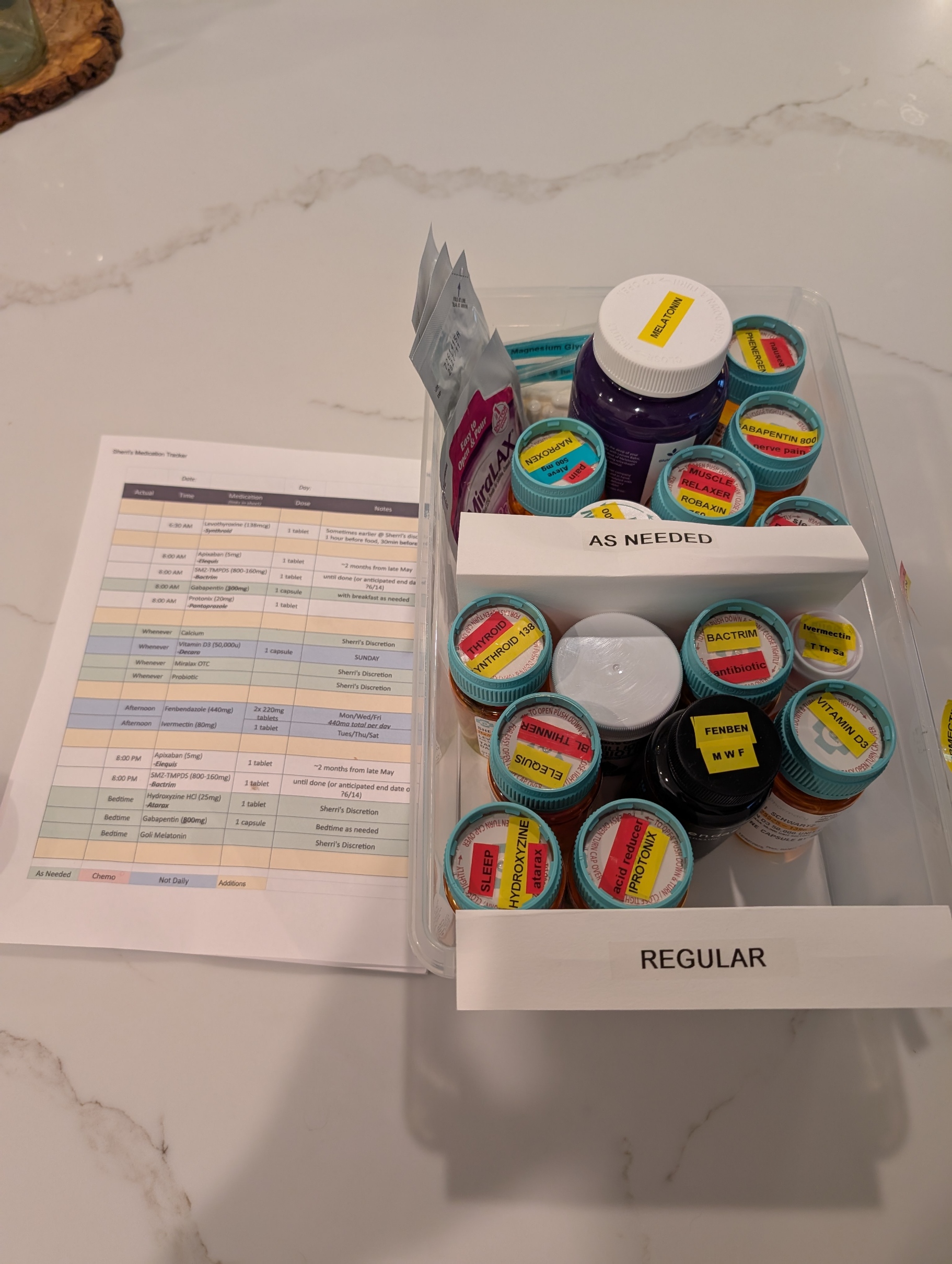
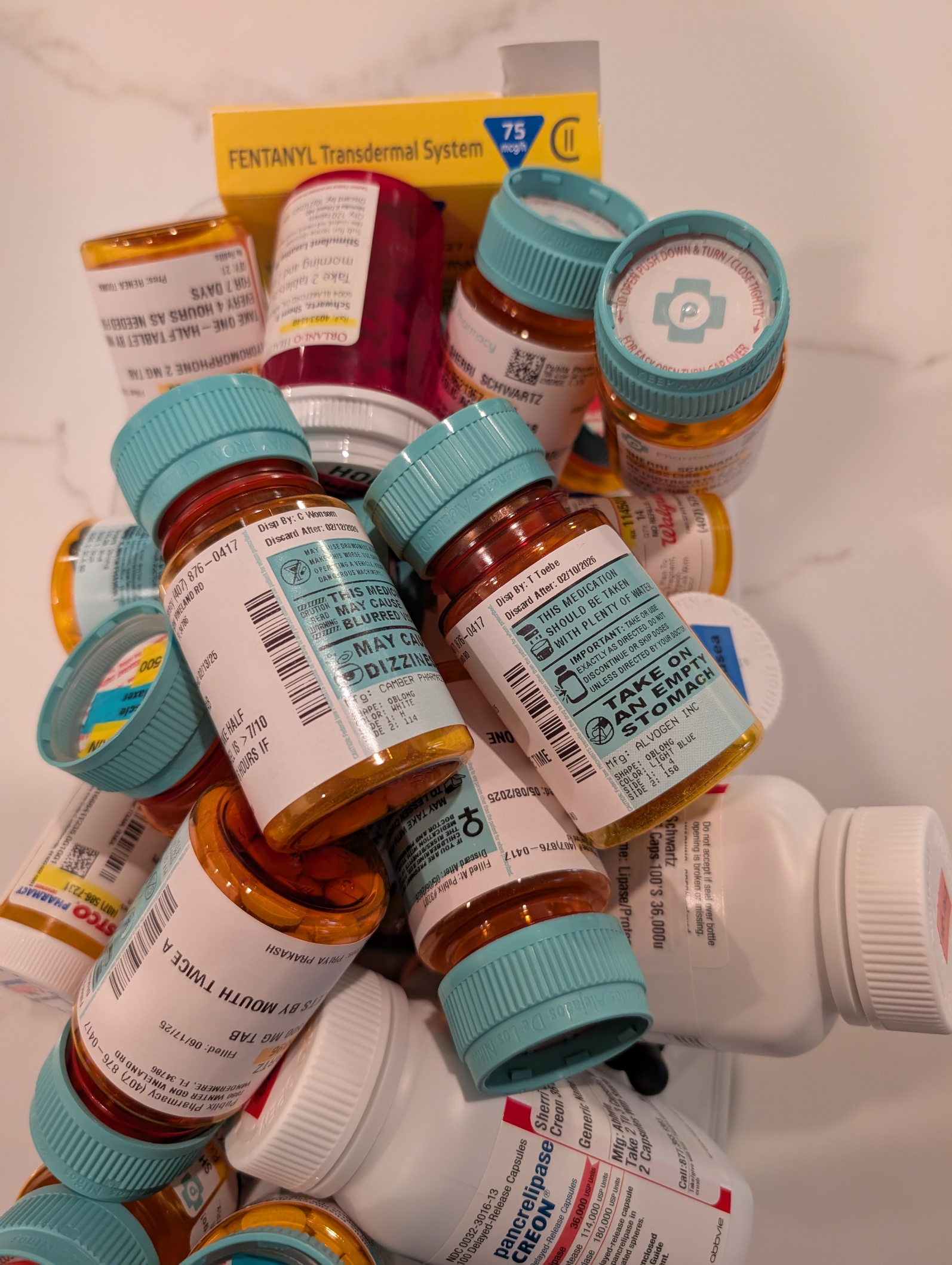
Pills, Pills, and More Pills: The Hidden Burden of Complex Caregiving
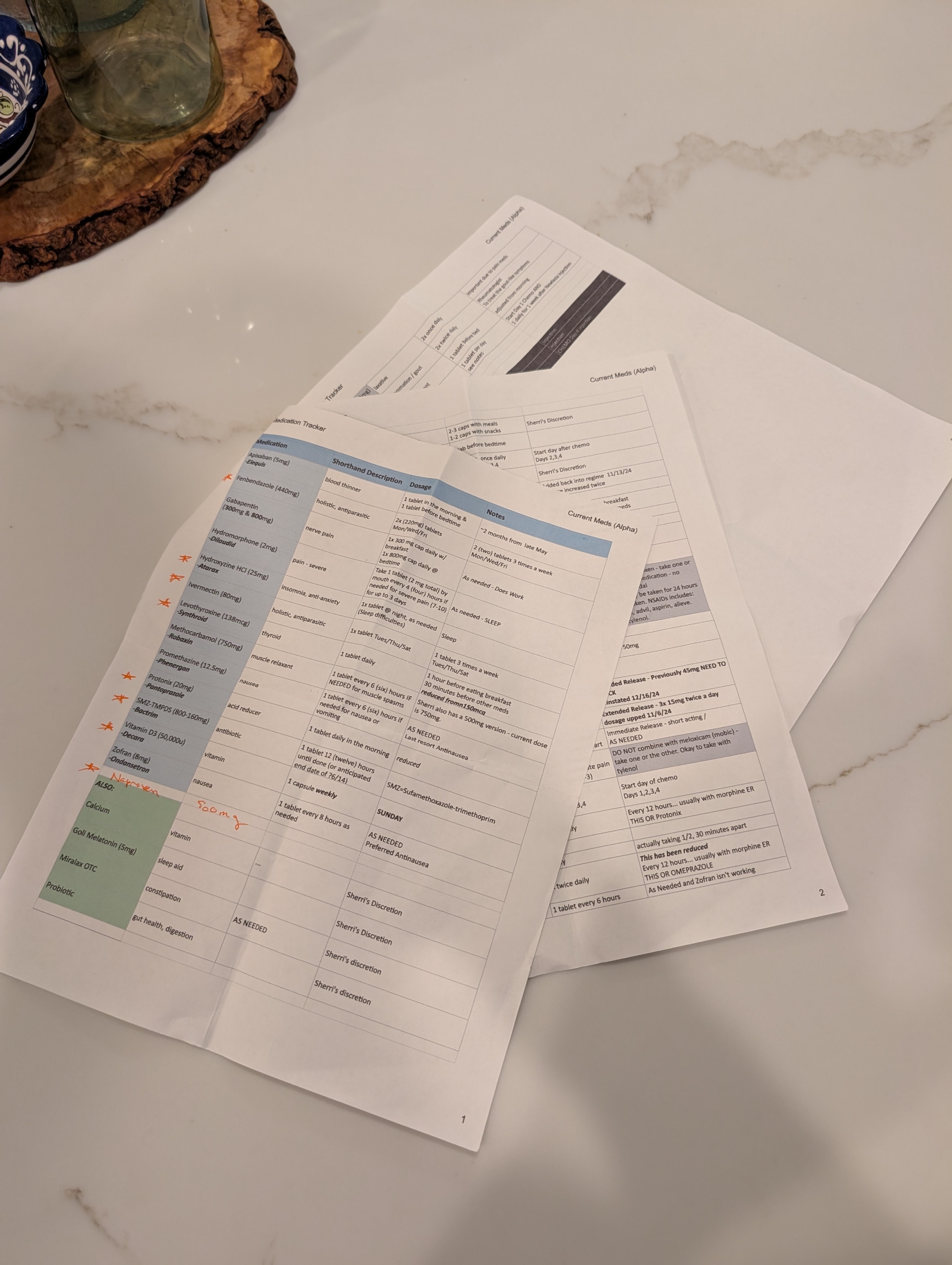
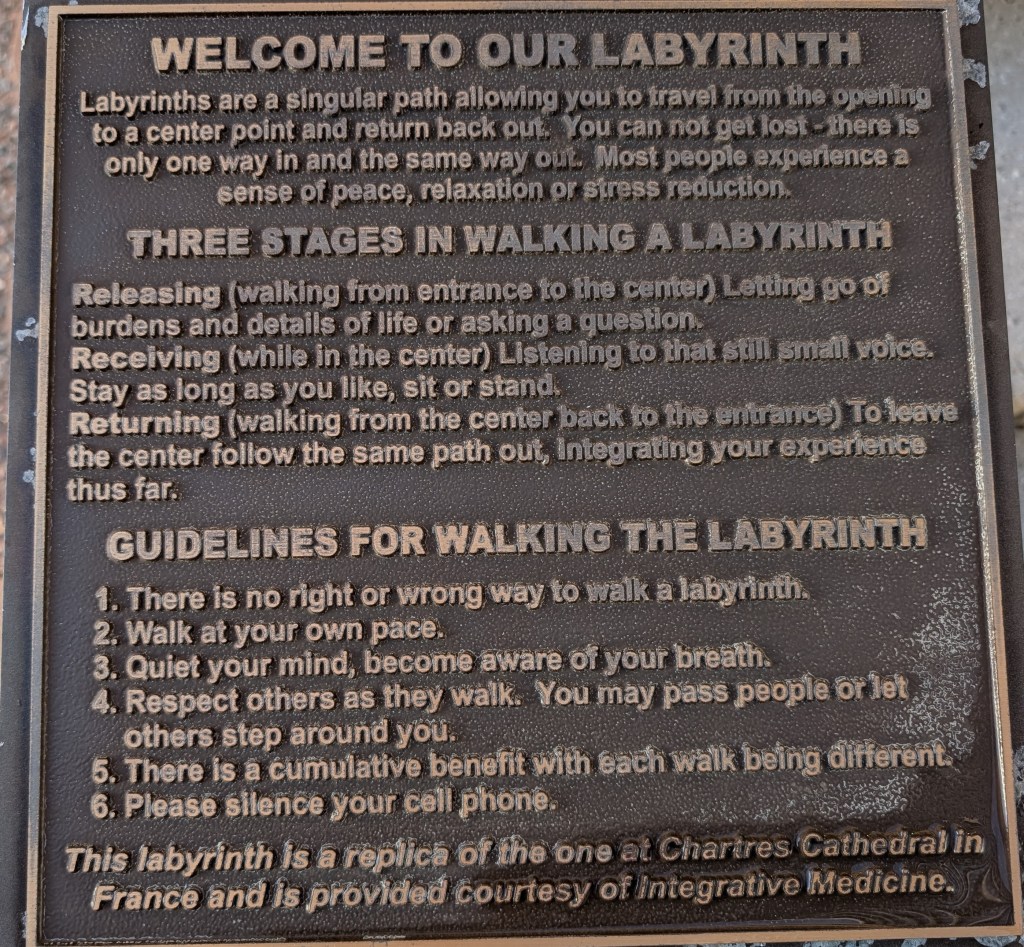
One of the most overwhelming challenges in being a caregiver to a loved one with complex health needs is managing medications. It’s not just about handing over a pillbox. It’s navigating a labyrinth of prescriptions from multiple providers—some within the same healthcare system, others outside it, and even some who are technically in the system but don’t have credentials to see each other’s records. The result? A fragmented network of well-meaning professionals relying on the patient or caregiver to connect the dots.
Every outpatient visit starts with the same question: “Are you still taking…?” And if your loved one isn’t completely lucid or you’re not fully dialed in 24/7, the answer might not be accurate. That’s when the real risk begins. Medications get missed, taken at the wrong time, or worse—interact dangerously. Even with tools like MyChart and pharmacy alerts, medication management for multi-disciplinary patients is a full-time job that demands vigilance and coordination.
Thankfully, my wife has what many don’t: an extended family care team. Her sister—a brilliant organizer—maintains a shared medication log with active and retired prescriptions. Her cousin, a provider based in California, monitors her records through MyChart and flags potential issues or treatment recommendations. Their support has been nothing short of lifesaving.
As her primary caregiver, I also leaned into my background in healthcare and team leadership. I applied principles I once used to support the care for wounded or sick soldiers returning from Iraq at Fort Moore (then Fort Benning), where we built systems but more importantly had people to prevent our service members from getting lost in the shuffle. It’s painful to see that the civilian system still struggles with the same problem.
Where is the care manager? Aren’t they the quarterback? I once asked that question myself—only to be told their panel included 250 complex cases. No human can meaningfully manage that many lives. It was a sobering reminder that “the system” is overloaded, and for those without advocates, the consequences can be tragic.
Having a palliative care physician onboard has been critical. Contrary to common perception, they don’t just deal with end-of-life care. They focus on quality of life—managing pain, coordinating care, and yes, reconciling all those pills. My wife currently has more than 10 providers involved in her care. That number doesn’t include staff, specialists, or the relentless demands of insurance approvals.
Medication management isn’t glamorous, but it’s a battlefield—and like all battlefields, it requires a team, a plan, and an unwavering commitment to the person you’re fighting for. I bring my military mindset to this mission every day. And while I can’t stop the tide of prescriptions or the systemic gaps in care, I can make sure my wife never faces them alone.