Blog Archives
Profits Over Patients: Why the Insurance System is Failing Families
The health insurance industry has mastered one thing above all else: delay. What should be a simple claim submission turns into months of bureaucratic limbo, hidden behind jargon like “not yet built” or “waiting for processing.” These phrases disguise the truth—that while families wait for critical financial support, corporations sit comfortably on record-breaking profits.
We are told to expect 15 business days just for a claim to be reviewed, then another 30 to 60 days for processing. In the meantime, representatives admit that claims often sit in inboxes, unseen, until patients themselves call to shake the system awake. And yet these same companies proudly announce hundreds of millions in net income, raising their performance outlooks. The disconnect could not be starker: efficiency for shareholders, inefficiency for patients.
This is not a matter of capability. If profits can soar, systems can be fixed. More staff can be hired. Processes can be modernized. But the lack of urgency shows where priorities lie. Patients and families are left to wait, wonder, and absorb the financial strain—all while the corporations built to serve them choose margin over mission.
And this isn’t an abstract critique. This is personal. The claim in question was for my wife’s electric wheelchair—a necessity, not a luxury—purchased on June 9th. It cost more than $2,000. I wrote about it on June 23rd in my blog post “In the Blink of an Eye: Grace in the Midst of the Unthinkable”, where I shared how something as simple as mobility could restore dignity in the midst of suffering. Months later, the claim has still not been processed. Letters arrive contradicting what agents say, and the only reason any progress happens is because I chase it down.
For families like mine, these delays aren’t just numbers on a balance sheet. They are nights spent worrying, bills that pile up, and faith that slowly erodes. Representatives on the front line may show compassion, but they are trapped in a system designed to stall. Until the industry prioritizes people over profit, these “micro” frustrations will continue to echo the much larger, systemic failure of our healthcare system.
You can read the June 23rd post here: In the Blink of an Eye: Grace in the Midst of the Unthinkable

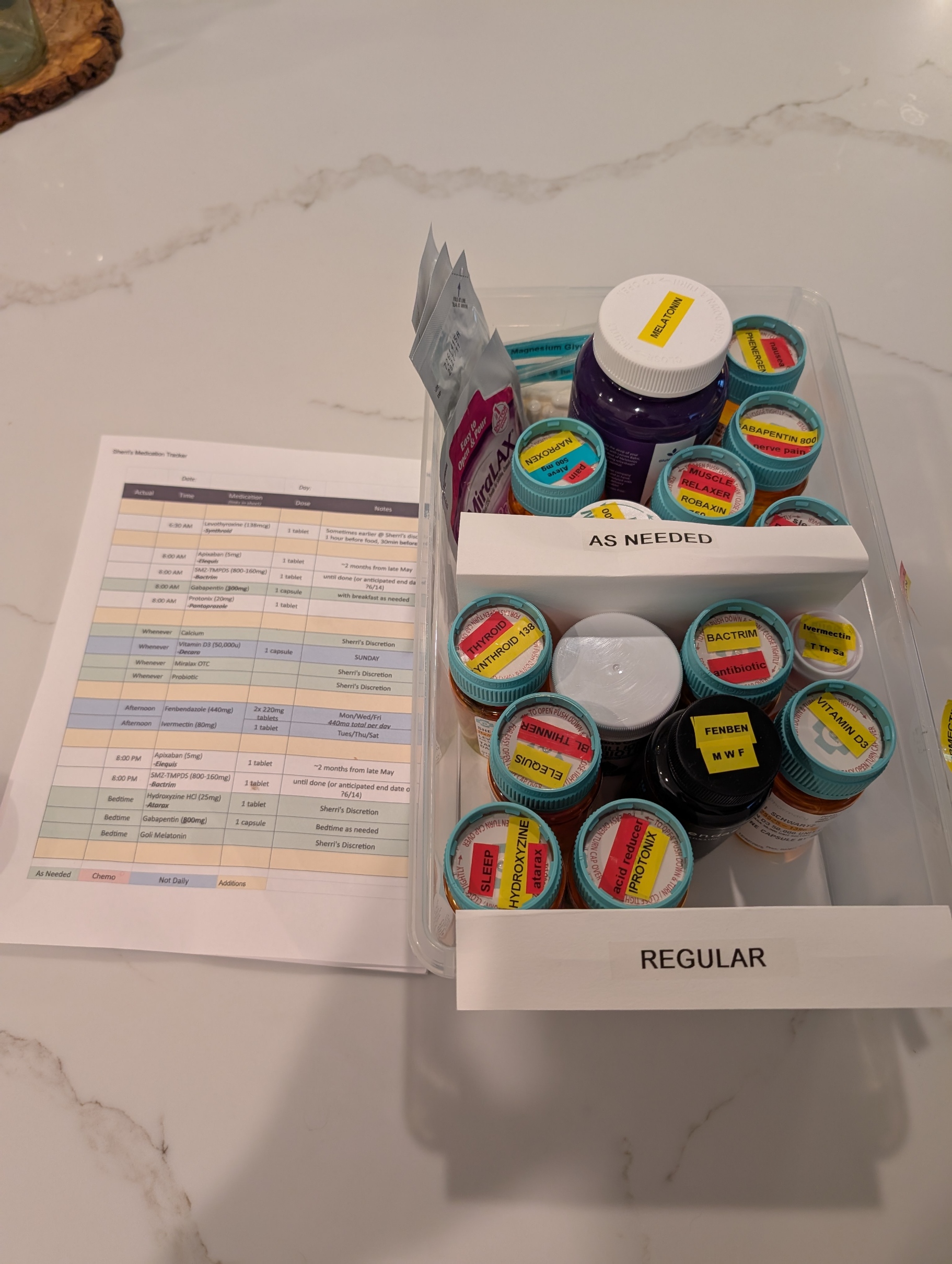
Pills, Pills, and More Pills: The Hidden Burden of Complex Caregiving
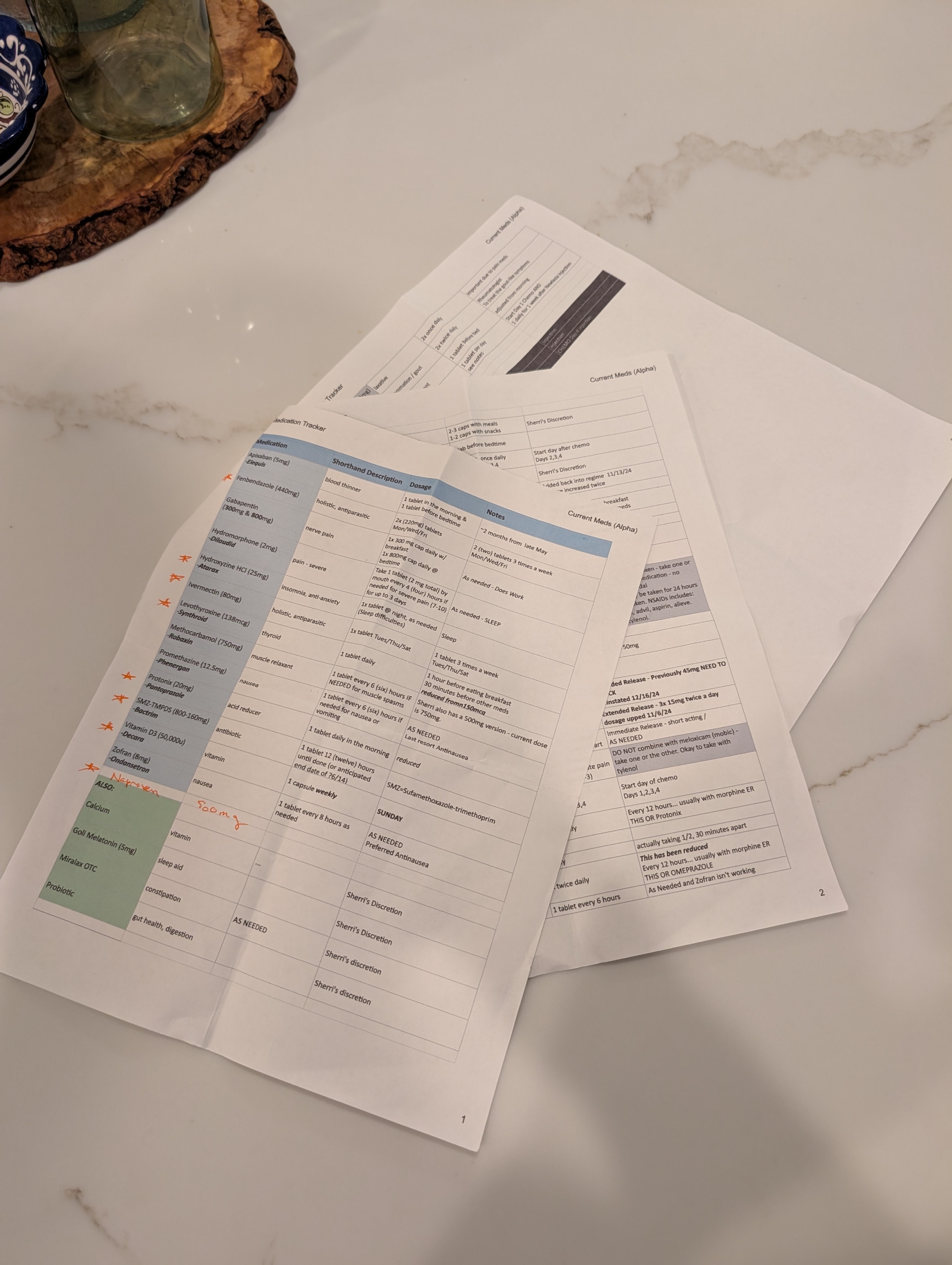
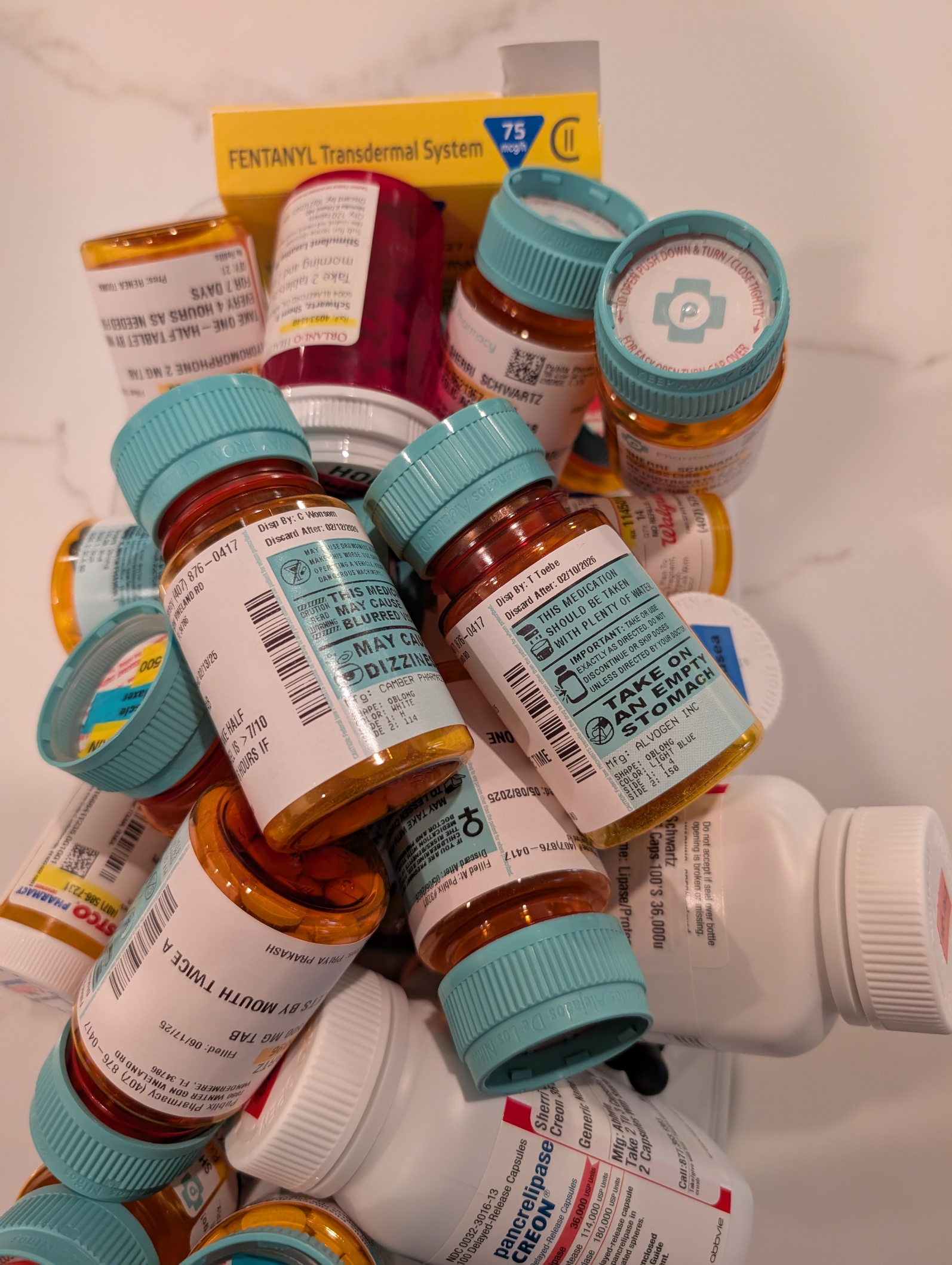
One of the most overwhelming challenges in being a caregiver to a loved one with complex health needs is managing medications. It’s not just about handing over a pillbox. It’s navigating a labyrinth of prescriptions from multiple providers—some within the same healthcare system, others outside it, and even some who are technically in the system but don’t have credentials to see each other’s records. The result? A fragmented network of well-meaning professionals relying on the patient or caregiver to connect the dots.
Every outpatient visit starts with the same question: “Are you still taking…?” And if your loved one isn’t completely lucid or you’re not fully dialed in 24/7, the answer might not be accurate. That’s when the real risk begins. Medications get missed, taken at the wrong time, or worse—interact dangerously. Even with tools like MyChart and pharmacy alerts, medication management for multi-disciplinary patients is a full-time job that demands vigilance and coordination.
Thankfully, my wife has what many don’t: an extended family care team. Her sister—a brilliant organizer—maintains a shared medication log with active and retired prescriptions. Her cousin, a provider based in California, monitors her records through MyChart and flags potential issues or treatment recommendations. Their support has been nothing short of lifesaving.
As her primary caregiver, I also leaned into my background in healthcare and team leadership. I applied principles I once used to support the care for wounded or sick soldiers returning from Iraq at Fort Moore (then Fort Benning), where we built systems but more importantly had people to prevent our service members from getting lost in the shuffle. It’s painful to see that the civilian system still struggles with the same problem.
Where is the care manager? Aren’t they the quarterback? I once asked that question myself—only to be told their panel included 250 complex cases. No human can meaningfully manage that many lives. It was a sobering reminder that “the system” is overloaded, and for those without advocates, the consequences can be tragic.
Having a palliative care physician onboard has been critical. Contrary to common perception, they don’t just deal with end-of-life care. They focus on quality of life—managing pain, coordinating care, and yes, reconciling all those pills. My wife currently has more than 10 providers involved in her care. That number doesn’t include staff, specialists, or the relentless demands of insurance approvals.
Medication management isn’t glamorous, but it’s a battlefield—and like all battlefields, it requires a team, a plan, and an unwavering commitment to the person you’re fighting for. I bring my military mindset to this mission every day. And while I can’t stop the tide of prescriptions or the systemic gaps in care, I can make sure my wife never faces them alone.