Pills, Pills, and More Pills: The Hidden Burden of Complex Caregiving
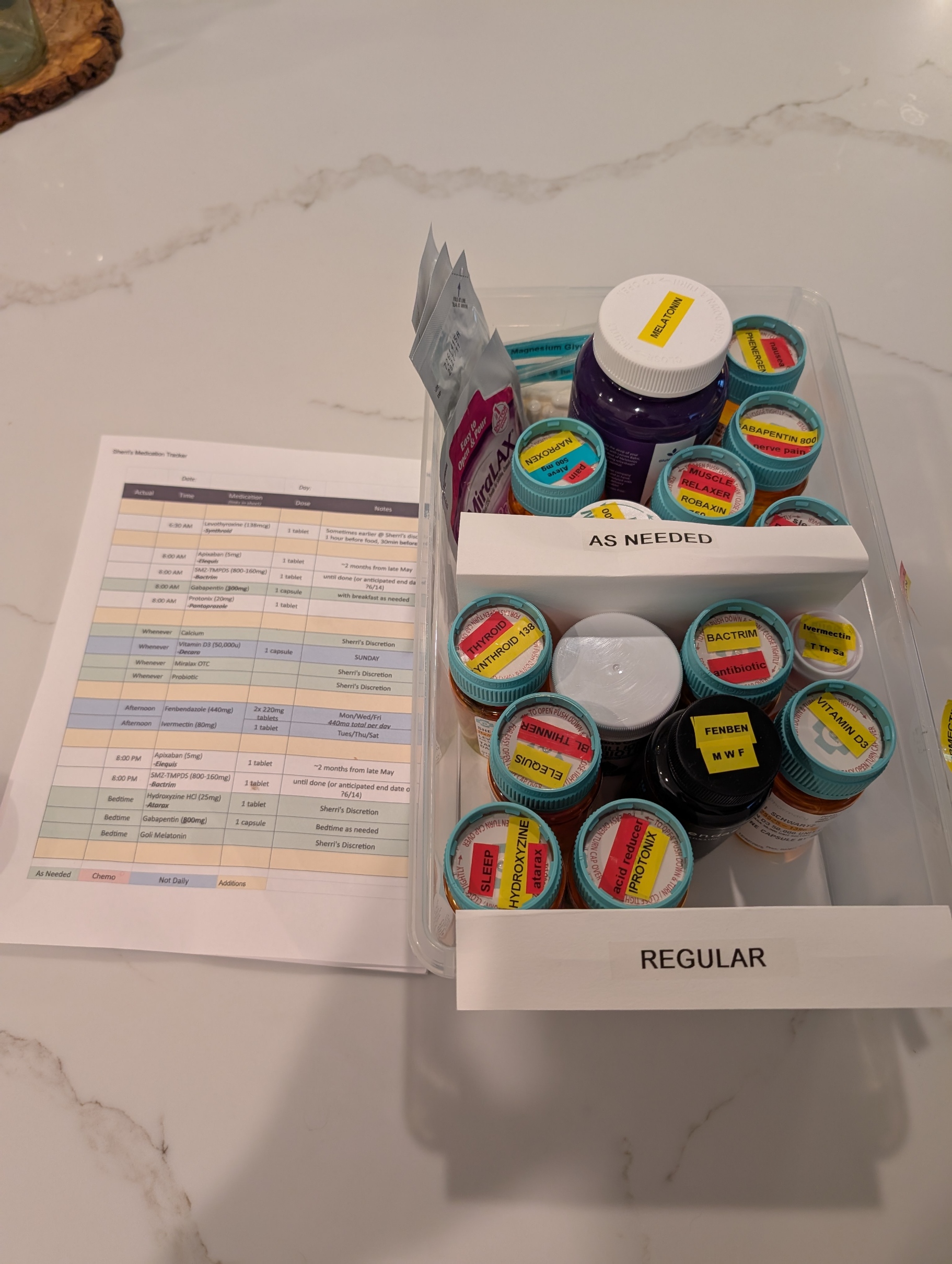
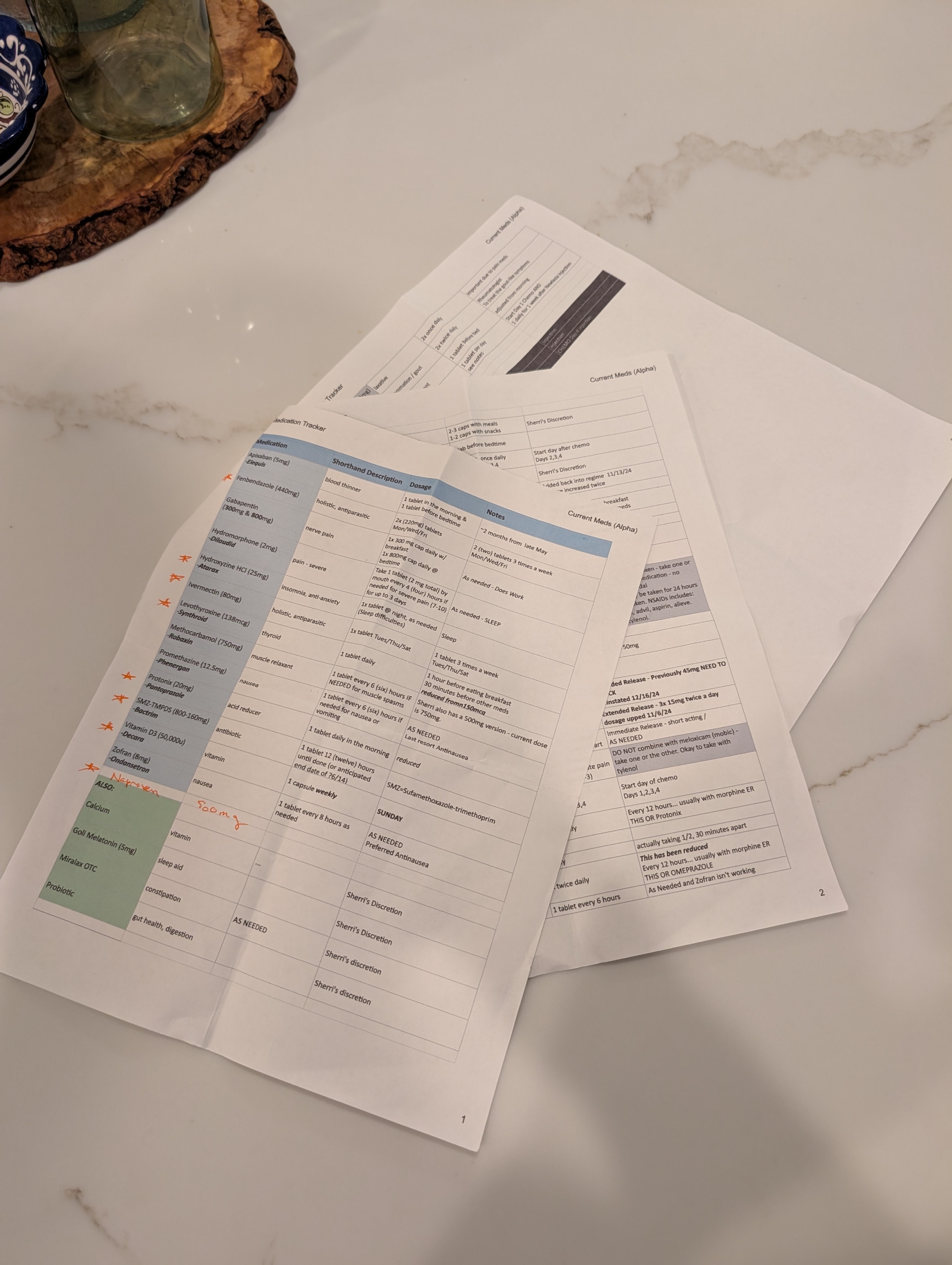
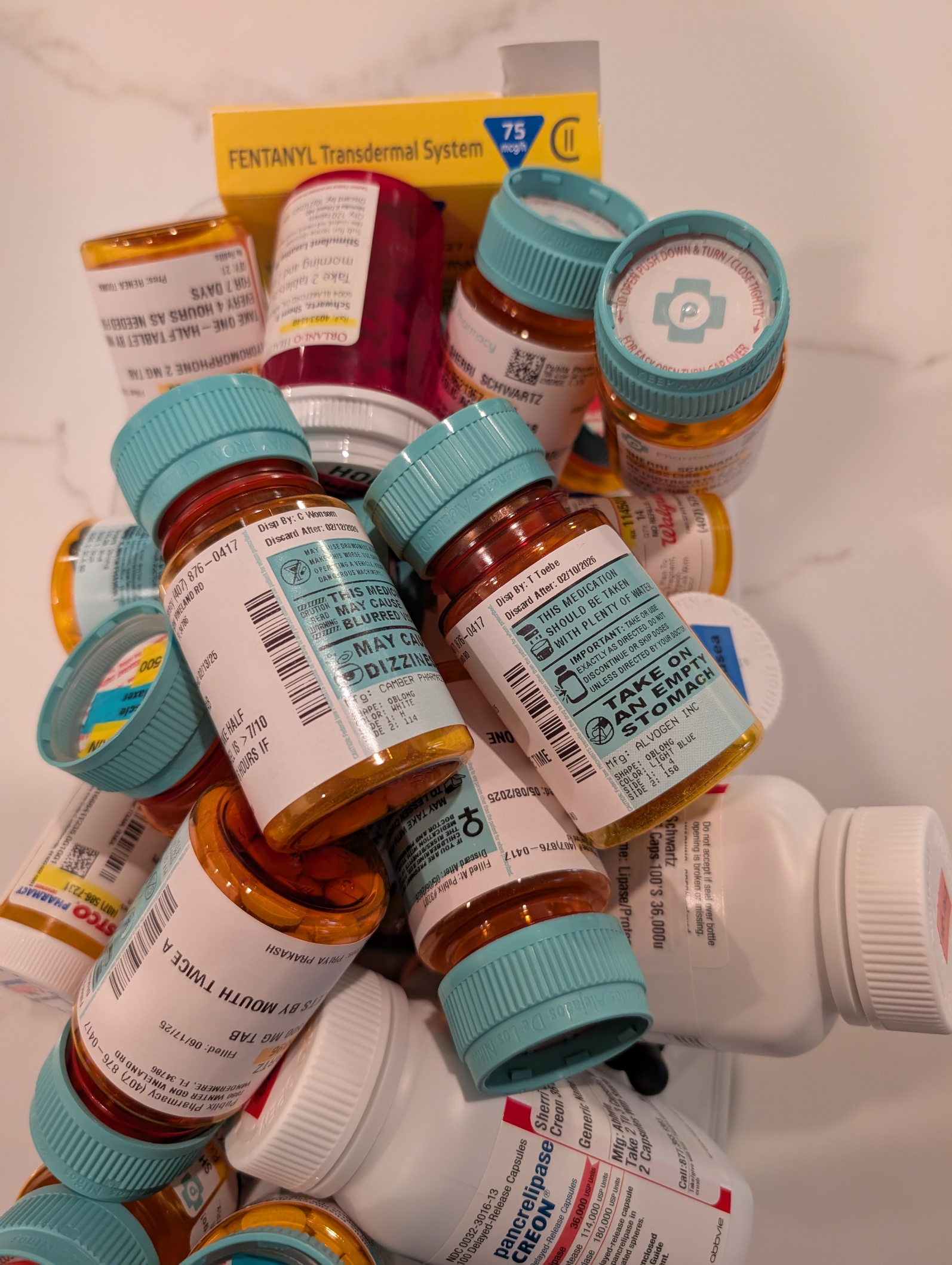
One of the most overwhelming challenges in being a caregiver to a loved one with complex health needs is managing medications. It’s not just about handing over a pillbox. It’s navigating a labyrinth of prescriptions from multiple providers—some within the same healthcare system, others outside it, and even some who are technically in the system but don’t have credentials to see each other’s records. The result? A fragmented network of well-meaning professionals relying on the patient or caregiver to connect the dots.
Every outpatient visit starts with the same question: “Are you still taking…?” And if your loved one isn’t completely lucid or you’re not fully dialed in 24/7, the answer might not be accurate. That’s when the real risk begins. Medications get missed, taken at the wrong time, or worse—interact dangerously. Even with tools like MyChart and pharmacy alerts, medication management for multi-disciplinary patients is a full-time job that demands vigilance and coordination.
Thankfully, my wife has what many don’t: an extended family care team. Her sister—a brilliant organizer—maintains a shared medication log with active and retired prescriptions. Her cousin, a provider based in California, monitors her records through MyChart and flags potential issues or treatment recommendations. Their support has been nothing short of lifesaving.
As her primary caregiver, I also leaned into my background in healthcare and team leadership. I applied principles I once used to support the care for wounded or sick soldiers returning from Iraq at Fort Moore (then Fort Benning), where we built systems but more importantly had people to prevent our service members from getting lost in the shuffle. It’s painful to see that the civilian system still struggles with the same problem.
Where is the care manager? Aren’t they the quarterback? I once asked that question myself—only to be told their panel included 250 complex cases. No human can meaningfully manage that many lives. It was a sobering reminder that “the system” is overloaded, and for those without advocates, the consequences can be tragic.
Having a palliative care physician onboard has been critical. Contrary to common perception, they don’t just deal with end-of-life care. They focus on quality of life—managing pain, coordinating care, and yes, reconciling all those pills. My wife currently has more than 10 providers involved in her care. That number doesn’t include staff, specialists, or the relentless demands of insurance approvals.
Medication management isn’t glamorous, but it’s a battlefield—and like all battlefields, it requires a team, a plan, and an unwavering commitment to the person you’re fighting for. I bring my military mindset to this mission every day. And while I can’t stop the tide of prescriptions or the systemic gaps in care, I can make sure my wife never faces them alone.
Posted on June 20, 2025, in Caregving, and tagged #caregiving, chronic-pain, health, healthcare, life, mental-health. Bookmark the permalink. Leave a comment.


Leave a comment
Comments 0